
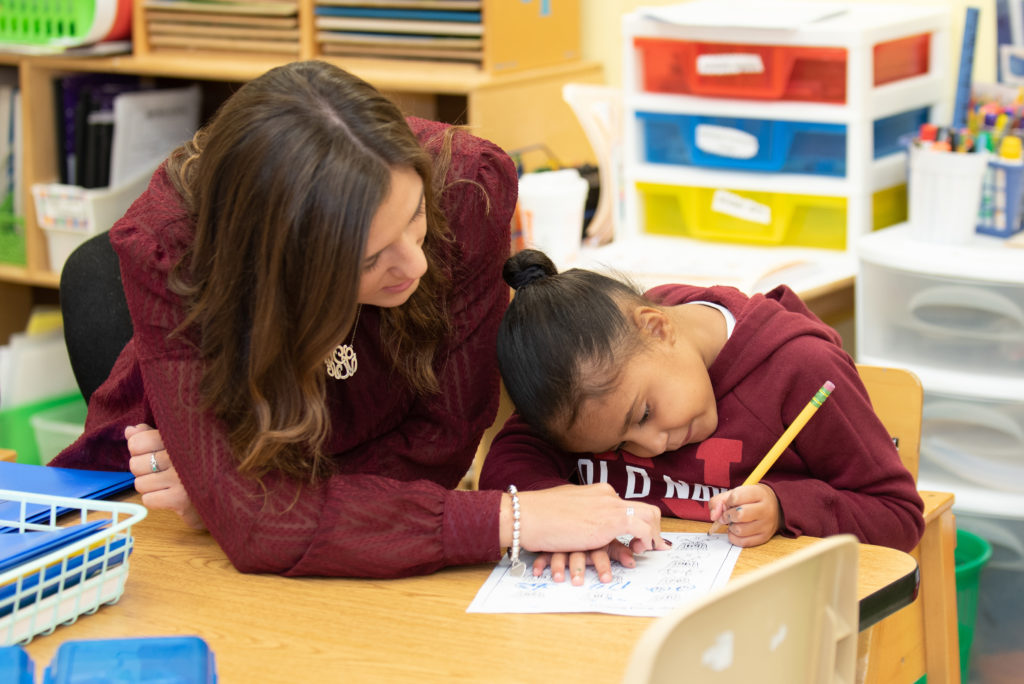
On any given day, First Children Services touches the lives of more than 1,000 children and families with a dedicated workforce of over 500 teachers, therapists, paraprofessionals and support staff.

What makes our approach different at First Children?
First Children Services is an equal opportunity employer and provider. Our agency prohibits discrimination and harassment of any type without regard to race, color, religion, age, sex, national origin, disability status, genetics, protected veteran status, sexual orientation, gender identity or expression, or any other characteristic protected by federal, state or local laws. All individuals featured on our website and social media have expressed written photo consent.